What Is Colon (Colorectal) Cancer?
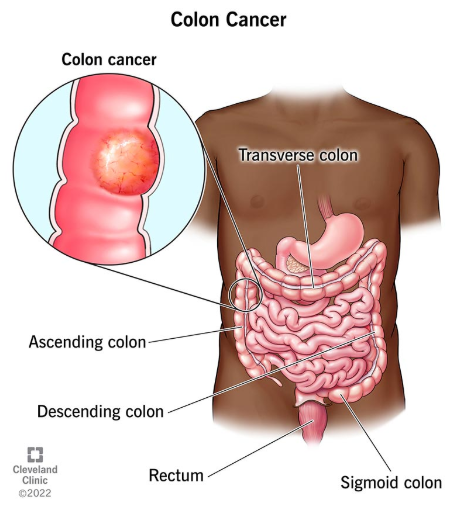
Colon cancer is a disease in which abnormal cells grow in the colon (large intestine). It is often caused by changes in the DNA of colon cells. These cells multiply without control and form tumors. It is usually found in older adults, but younger people can be affected too. In many cases, it begins as small, noncancerous polyps. Over time, some of these polyps may turn into cancer. The disease is often silent in the early stages. It may be detected during routine screenings. If left untreated, it can spread to other parts of the body.
Symptoms?
- Persistent Diarrhea: Frequent loose, watery stools lasting more than a few days may signal a bowel health change, possibly linked to colon cancer.
- Chronic Constipation: Long-term difficulty passing stool or infrequent bowel movements could suggest a colon obstruction from a tumor.
- Blood on the Rectum: Bright red blood after a bowel movement may indicate rectal bleeding, a possible colon cancer sign.
- Blood in the Stool: Dark or tar-like stool could mean internal bleeding in the digestive tract.
- Thin, Ribbon-Like Stools: Narrow stools may point to a colon obstruction or narrowing.
- Constant Bowel Urge: Feeling the need to pass stool even when empty may suggest colon or rectal irritation.
- Incomplete Bowel Emptying: The sensation of not fully emptying the bowels could signal a blockage or tumor.
- Abdominal Cramping or Bloating: Ongoing discomfort, cramps, or bloating may relate to colon cancer-related bowel changes.
- Unexplained Weight Loss or Fatigue: Sudden weight loss without diet changes, along with persistent fatigue, may indicate the body is fighting cancer.
Symptoms in women:
While colorectal cancer symptoms are similar for men and women, women may mistake them for menstrual, menopausal, or common digestive issues. Because of this, they should pay extra attention to these warning signs:
- Abdominal Discomfort – Persistent cramping, bloating, or pain unrelated to your menstrual cycle could signal colon cancer.
- Changes in Bowel Habits – Diarrhea, constipation, or irregular bowel movements lasting more than a few days should not be ignored.
- Unexplained Fatigue – Constant tiredness without a clear cause may indicate an underlying issue like colon cancer.
- Rectal Bleeding or Blood in Stool – Any blood in stool or from the rectum should be checked by a doctor immediately.
- Unexplained Weight Loss – Losing weight without diet or exercise changes could be a red flag.
Since these symptoms can overlap with other conditions, women should stay alert and get regular screenings. Early detection greatly improves treatment success.

Causes:
Colon cancer develops when cells in the colon or rectum grow and multiply uncontrollably. Normally, cells in your body grow, divide, and die in a controlled way to keep tissues healthy. But in colon cancer, these cells don’t die when they should, forming tumors. Many cases start as small growths called polyps, which can turn cancerous over time.
While the exact reason some polyps become cancerous is unknown, certain risk factors increase the chances. These include medical conditions (like inherited syndromes) and lifestyle habits. Having risk factors doesn’t guarantee cancer, but it means you should be more aware and discuss screening with a doctor. Early detection can make a big difference in treatment success.
Stages:
Colorectal cancer is staged based on how far it has spread and the size of the tumor. The stages help determine the best treatment options.
- Stage 0 (Carcinoma in Situ): The earliest stage, where cancer is only in the inner lining of the colon. It is highly treatable.
- Stage 1: The cancer has grown into deeper layers of the colon wall but hasn’t spread further.
- Stage 2: Cancer has reached the outer layers of the colon but has not spread outside it.
- Stage 3: Cancer has grown through the colon wall and spread to nearby lymph nodes but not to distant organs.
- Stage 4: The most advanced stage, where cancer has spread beyond the colon to other organs (such as the liver or lungs).
As the stage increases, the cancer becomes more advanced and harder to treat. Early detection improves treatment success.

Risk Factors:
Several lifestyle choices can increase your risk of colon cancer. Here’s what you should know:
- Smoking: Tobacco products—including cigarettes, chewing tobacco, and e-cigarettes—raise your risk of colon cancer.
- Excessive alcohol: Drinking too much alcohol increases your risk. Men should limit alcohol to two drinks per day, while women should stick to one drink per day. Even light drinking can contribute to cancer risk.
- Obesity: A diet high in fat and calories can lead to weight gain, which raises your risk.
- Red and processed meats: Eating too much bacon, sausage, deli meats, and other processed meats may increase your risk. Experts recommend limiting these to no more than two servings per week.
- Lack of exercise: Regular physical activity—even in small amounts—can help lower your risk.
By making healthier choices, you can reduce your chances of developing colon cancer.
Health Conditions That Raise Colon Cancer Risk
Certain health conditions and genetic factors can increase your risk:
- Inflammatory bowel disease (IBD): Chronic conditions like ulcerative colitis and Crohn’s disease cause long-term colon inflammation, raising cancer risk—especially if present for over seven years or affecting large areas.
- Inherited syndromes: Genetic disorders like Lynch syndrome and familial adenomatous polyposis (FAP) significantly increase colon cancer risk.
- Family history of colon cancer: Having a parent, sibling, or child with colon cancer raises your risk, particularly if they were diagnosed before age 45.
- Family history of advanced polyps: If a close relative had large or precancerous polyps, your risk increases.
- Multiple polyps: People with many colon polyps (adenomas, serrated polyps, etc.) or inherited polyp syndromes face higher cancer risk.
Diagnosis:
Doctors use several tests to check for colon cancer:
1. Complete Blood Count (CBC): Checks for anemia or infection.
2. Comprehensive Metabolic Panel (CMP): Evaluates liver and kidney function.
3. CEA Assay: Measures a protein (CEA) that may be high in colon cancer.
4. Imaging Tests:
- X-rays, CT, MRI, or PET scans: Create detailed images to locate tumors.
- Ultrasound: Uses sound waves to examine tissues.
5. Biopsy: Removes a small tissue sample to confirm cancer.

Treatments
Treatment depends on cancer stage and patient health. Main options:
1. Surgery
- Removes tumors (polypectomy for small growths, colectomy for larger areas)
- May require a stoma if colon can’t be reconnected
- Also used to relieve symptoms in advanced cases
2. Immunotherapy
- Boosts immune system to fight cancer
- Uses drugs like Keytruda or Opdivo
- Can cause fatigue, rash, or (rarely) serious immune reactions
3. Chemotherapy
- Kills fast-growing cancer cells
- Used before/after surgery or for spread cancer
- Side effects include nausea and hair loss
4. Radiation
- Targets cancer with high-energy beams
- Mainly for rectal cancer or metastatic tumors
- May cause temporary skin irritation or fatigue
Prevention
While there’s no surefire way to prevent colon cancer, you can significantly reduce your risk through these evidence-based strategies:
Lifestyle Prevention:
- Maintain a healthy weight through balanced nutrition
- Stay physically active with regular exercise
- Eat a diet rich in fruits, vegetables and whole grains
- Limit red meat and processed foods high in saturated fats
- Moderate alcohol consumption and avoid tobacco completely
Early Detection is Key:
Since colon cancer often develops without symptoms initially, screening is crucial. Medical experts recommend:
- Starting regular screenings at age 45 (earlier for high-risk individuals)
- Annual fecal immunochemical tests (FIT) to detect blood in stool
- Flexible sigmoidoscopy every 5 years to examine the lower colon
Your ideal screening schedule depends on personal risk factors like family history. Consult your doctor to create a personalized prevention and screening plan. Remember, early detection through screening can prevent cancer development and dramatically improve outcomes when caught early.
FAQs
1. Could your unexplained fatigue or bloating be warning signs of colorectal cancer?
While occasional digestive issues are normal, persistent symptoms like chronic constipation/diarrhea, pencil-thin stools, or rectal bleeding could signal colon cancer – especially if accompanied by unexplained weight loss or fatigue. Women often mistake these signs for menstrual or menopause symptoms, delaying diagnosis. Since early-stage colon cancer frequently has no symptoms at all, don’t wait for warning signs. Screening starting at 45 (earlier if high-risk) can detect precancerous polyps before they turn cancerous.
2. Is colon cancer preventable? Here’s what doctors want you to know.
While not 100% preventable, up to 75% of colon cancer cases could be avoided through lifestyle changes and screening. Key defenses:
- Diet & Exercise: Swap processed meats for fiber-rich foods and stay active
- Avoid Risks: Quit smoking and limit alcohol
- Genetic Awareness: Know your family history – Lynch syndrome and other inherited conditions multiply risk
- Screening Saves Lives: Colonoscopies can both detect and remove precancerous growths during the same procedure




